‘No magic bullet:’ Colorado officials seek ways to curb rising Medicaid costs
Colorado’s Medicaid costs are outpacing the state’s revenue and spending limits imposed by TABOR, forcing discussions around how to rein in health care spending

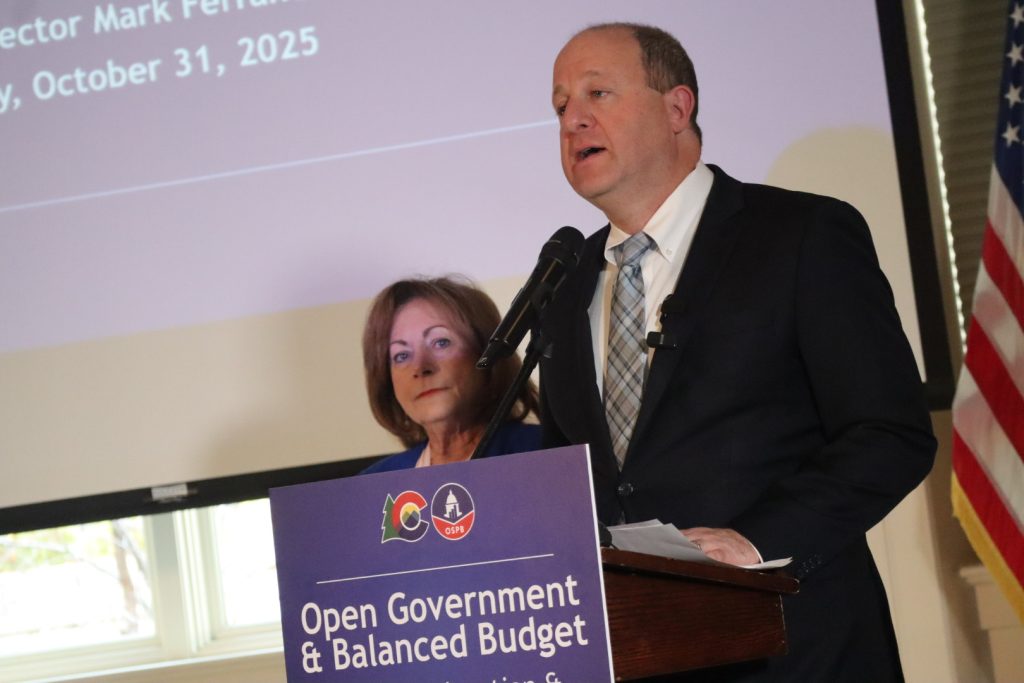
John F. Russell/Steamboat Pilot & Today
Colorado’s spending on Medicaid — the federal-state program that covers more than 1 in 5 low-income Coloradans — is reaching a point of unsustainability, state officials say.
Cuts to the program may be on the horizon, and those decisions are likely to dominate budget conversations in 2026, as state lawmakers return to the Capitol for another legislative session.
Gov. Jared Polis’ office is seeking measures to reduce Medicaid spending by roughly half of what it was projected to be next fiscal year, though many of the office’s proposals have been met with skepticism from the Joint Budget Committee, the group of lawmakers tasked with writing the budget that will be voted on by the legislature this spring.
As discussions around Medicaid unfold, officials are digging deeper into some of its largest cost drivers and ideas for how to slow spending.
“There is no magic bullet. I think we all wish that there were,” said Melinda Dutton with Manatt Health, a consulting firm that compiled a recent report on Colorado’s Medicaid spending.
Dutton and others presented the findings of that report during a Dec. 18 virtual webinar. They were joined by the head of the governor’s budget office and officials with the Colorado Department of Health Care Policy and Financing, the agency that oversees the state’s Medicaid program.
Dutton said the goals of the analysis are to find ways to temper the program’s costs while preserving access to core services.
“You can take a hatchet to the program and damage its underlying purpose,” Dutton said, “or, you can take a scalpel and really look for value in the program, and that’s what we’re focused on.”
The Manatt report highlights that Colorado is not an outlier when it comes to escalating Medicaid costs. That’s due primarily to health care costs outpacing wages and increased enrollment, much of which occurred during the COVID-19 pandemic.
“All states are struggling with their Medicaid budgets,” Dutton said.
Dutton added that despite growing costs, Medicaid remains the least expensive form of health coverage in the U.S. and is significantly cheaper to provide compared to Medicare, which covers people over age 65, or private insurance.
The report found that since fiscal year 2018, spending on the state’s Medicaid program has risen by nearly 60%, representing a roughly 8% increase per year.
That’s almost double the rate of the state’s revenue growth cap, which comes from the Taxpayer’s Bill of Rights, or TABOR. The 1992 voter-approved amendment to the Colorado Constitution limits state revenue to the rate of population growth plus inflation. Any excess revenue must be returned to taxpayers.
TABOR is a system unique to Colorado, and some state leaders have grown increasingly frustrated with the limitations it puts on spending for government services.
Mark Ferrandino, who leads the governor’s Office of State Planning and Budgeting, said Polis has supported past efforts to overhaul TABOR. That includes Proposition CC, a 2019 ballot measure that would have abolished the state’s revenue cap, which voters ultimately rejected.
More recently, some state lawmakers proposed a lawsuit last year to try to invalidate TABOR as unconstitutional. The measure failed to gain enough traction in the legislature, and Polis did not publicly weigh in on the measure.

Most attempts to reform TABOR, however, have had to go before voters, who are required to approve any state changes that raise taxes.
“I know there continue to be conversations on different policy options to either raise revenue or adjust the (TABOR) cap at the legislature,” Ferrandino said. “Ultimately, all of those questions come back to the voters, who have to decide that.”
Another factor amplifying Colorado’s Medicaid pressures is the state’s lower share of federal funding.
The federal government splits the cost of Medicaid with states, covering as much as 80% of the program’s costs in the poorest states. Because Colorado is a wealthier state, it has among the lowest ratios of federal funding nationally, with the federal government covering half of its Medicaid costs.
The report from Manatt found, however, that while Colorado receives less federal funding due to being a wealthier state, its TABOR constraints mean state spending is more closely aligned with poorer states.
Areas where the state’s Medicaid program has seen some of the largest cost increases include pharmaceutical drugs, expanded behavioral health services, and long-term care, partly driven by the state’s aging population.
When it comes to pharmaceuticals, just 2% of drugs covered under Medicaid account for 50% of the program’s drug costs, according to the Manatt report.
Colorado Department of Health Care Policy and Financing Executive Director Kim Bimestefer said that’s due to high-cost specialty drugs, whereas the cost of most generic drugs has remained fairly flat.
Bimestefer said the state has taken some action to rein in those costs, including eliminating the need for middlemen by signing contracts with drug manufacturers themselves, and seeking reimbursements from manufacturers when drugs don’t work or underperform.
But the state also needs federal intervention to help curb drug costs, including more price negotiations between the federal government and drug manufacturers and limits on drug makers’ patent extensions, Bimestefer said.
Dutton, the consultant with Manatt Health, added other recommendations for how Colorado can lower its Medicaid costs, including more tiered pricing for behavioral health services, rather than offering a flat rate.
Dutton stressed that the group’s recommendations are “very high level.”
“That’s a reflection of where we are in our process,” Dutton said, adding that there will be more input from stakeholders to hone recommendations.
The governor’s office, meanwhile, has already laid out its ideas for reducing Medicaid costs in its 2026-27 budget proposal before lawmakers.
Ideas include limiting billing hours for home health nursing and therapy services, reinstating a cap on adult dental benefits, and keeping provider reimbursement rates flat.
The governor’s budget office did not discuss those recommendations in depth during the December webinar, but Ferrandino, its director, acknowledged, “We made some tough decisions to slow the growth of Medicaid.”
“We know this is not an easy conversation,” he said.

Support Local Journalism

Support Local Journalism
Readers around Glenwood Springs and Garfield County make the Post Independent’s work possible. Your financial contribution supports our efforts to deliver quality, locally relevant journalism.
Now more than ever, your support is critical to help us keep our community informed about the evolving coronavirus pandemic and the impact it is having locally. Every contribution, however large or small, will make a difference.
Each donation will be used exclusively for the development and creation of increased news coverage.










